Introduction
You’ve probably heard that losing belly fat requires eating less and exercising more. But what if that advice is actually making your problem worse?
The truth is, not all belly fat is created equal. While the soft fat you can pinch under your skin is primarily a cosmetic concern, the fat wrapped around your liver, pancreas, and intestines—called visceral fat—is a metabolic time bomb. This fat is metabolically active, inflammatory, and directly linked to heart disease, type 2 diabetes, fatty liver disease, and metabolic dysfunction. The dangerous part? You can look relatively thin and still harbor dangerous levels of visceral fat.
Here’s what most people don’t realize: visceral fat accumulation isn’t fundamentally a calorie problem. It’s a hormonal signaling problem. Two hormones—insulin and cortisol—act as the master switches controlling where your body stores energy. When both remain chronically elevated, your body enters survival mode and protects visceral fat at all costs, regardless of how much you exercise or restrict calories.
This comprehensive guide reveals the science behind visceral fat, explains why traditional approaches often fail, and provides a proven hormonal framework for eliminating dangerous belly fat while preserving muscle, energy, and metabolic health.
Understanding Visceral Fat: Why It’s Different From Other Body Fat
The Hidden Danger Beneath Your Ribs
Most people conflate all belly fat, but visceral fat operates under completely different rules than subcutaneous fat (the pinchable fat under your skin). Visceral fat surrounds your vital organs like a metabolic parasite, and its behavior is fundamentally different from fat stored elsewhere on your body.
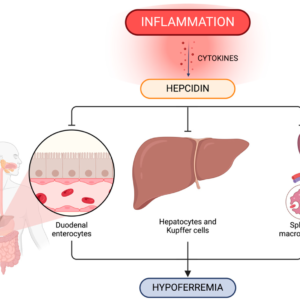
The distinction matters because visceral fat is metabolically active in ways that promote disease. It secretes inflammatory compounds called cytokines, increases insulin resistance, elevates blood pressure, and disrupts normal liver function. Research from the Mayo Clinic on visceral fat demonstrates that visceral fat accumulation correlates more strongly with metabolic disease than total body weight or BMI. A person can have a normal BMI and still suffer from visceral fat-related metabolic dysfunction.

Visceral vs. Subcutaneous Fat: Key Differences
| Factor | Visceral Fat | Subcutaneous Fat |
|---|---|---|
| Location | Wrapped around organs | Under skin, visible |
| Metabolic Activity | Highly active, inflammatory | Relatively inert |
| Health Risk | Directly linked to disease | Primarily cosmetic concern |
| Insulin Sensitivity | High density of insulin receptors | Fewer insulin receptors |
| Mobilization | Requires hormonal optimization | Mobilizes more easily |
| Response to Stress | Expands with cortisol elevation | Less cortisol-sensitive |
The insulin receptor density in visceral fat is significantly higher than in subcutaneous fat, which means visceral fat cells respond more aggressively to insulin signals. When insulin remains chronically elevated, visceral fat grows faster and is protected more fiercely by your body’s survival mechanisms. This explains why someone can have thin arms and legs while carrying a dangerous amount of abdominal fat.
The Insulin Problem: Why Calories Don’t Tell the Whole Story
Insulin Is the Master Storage Hormone
The conventional weight-loss narrative focuses obsessively on calories: eat less, move more, create a deficit. But this framework misses the fundamental driver of visceral fat accumulation—insulin.
Insulin is your body’s primary storage hormone. Every time insulin rises, fat burning shuts off completely. Not slows down—shuts off. As long as insulin remains elevated, your body cannot access stored fat, especially visceral fat. This is why someone can eat a low-calorie diet and still maintain high insulin levels all day long, keeping visceral fat locked in place.
The problem isn’t the total calories consumed—it’s the frequency and type of foods that trigger insulin spikes. Eating refined carbohydrates, sugars, or snacking every two to three hours keeps insulin chronically elevated. The pancreas never gets a break. The liver continuously converts excess glucose into fat, and that fat preferentially gets stored viscerally because visceral fat cells have a higher density of insulin receptors than subcutaneous fat cells.
The Silent Precursor: Insulin Resistance Before High Blood Sugar
Here’s what most people don’t know: insulin resistance doesn’t start when your blood sugar rises. It starts years earlier, when insulin levels remain chronically high while blood sugar still appears normal. During this silent phase, insulin is actively driving visceral fat accumulation, inflammation, and vascular damage. By the time your doctor finally flags elevated blood sugar, the metabolic damage is already extensive.
The fastest way to lower insulin isn’t exercise, supplements, or eating less food. It’s eating less often. Every time you eat, insulin rises. When you stop eating, insulin falls. This is basic physiology. If insulin never gets time to come down, fat burning never turns on.
The Cortisol Connection: Why Stress Creates Belly Fat
Cortisol: The Survival Hormone That Backfires
Cortisol is often vilified as “the stress hormone,” but this oversimplifies its role. Cortisol is actually a survival hormone designed to keep you alive during genuine emergencies by raising blood sugar, breaking down tissue, and mobilizing energy. This system works brilliantly in acute crises. It fails catastrophically when activated chronically.
When cortisol remains elevated day after day, your body behaves as if it’s under constant threat. In this state, fat loss becomes metabolically dangerous from your body’s perspective. Your nervous system interprets the signal as: “Danger is everywhere. Food is scarce. Conserve energy and protect reserves.” The body responds by protecting and even expanding visceral fat because visceral fat provides rapid energy access during perceived emergencies.
Cortisol directly raises blood sugar through a process called gluconeogenesis, where the liver produces glucose on demand. When blood sugar rises, insulin rises. This means chronic stress keeps insulin elevated even if you’re not eating much. The body is manufacturing sugar internally, and because that sugar didn’t come from food, people often blame age, hormones, or metabolism when the real culprit is cortisol-driven insulin resistance.
Major Cortisol Triggers Most People Ignore
Poor Sleep: Sleeping less than 6-7 hours per night elevates cortisol the following day. This triggers increased appetite, reduced insulin sensitivity, intensified cravings, and accelerated visceral fat storage. No diet can overcome chronic sleep deprivation.
Excessive Exercise: Exercise is a stress. In small, controlled doses, it improves insulin sensitivity. In excessive or prolonged doses—especially combined with caloric restriction—it raises cortisol and worsens visceral fat retention. This explains why endurance athletes often develop stubborn belly fat despite high activity levels.
Chaotic Fasting: Fasting is beneficial when done intentionally and calmly, but random, stressful fasting—especially combined with caffeine overload and poor sleep—signals danger to your body. The result is hormonal resistance, not fat loss.
Emotional Stress: Chronic anger, guilt, fear, and anxiety are interpreted by your nervous system as ongoing threats. These emotional states keep cortisol elevated even when everything else is optimized. This is why relaxation, forgiveness, laughter, and social connection aren’t soft recommendations—they’re metabolic interventions.
The Hormonal Solution: Restoring Insulin and Cortisol Balance
Time-Restricted Eating: The Safest Path to Lower Insulin
The goal with eating and fasting isn’t to punish your body—it’s to restore hormonal rhythm. When hormones follow their natural cycles, visceral fat loss happens almost automatically. When those rhythms are disrupted, no amount of effort can override the resistance.
Time-restricted eating (eating within a defined window and fasting the rest of the day) is one of the most effective and sustainable approaches. For most people, an 8-hour eating window works well. Some individuals thrive with a 6-hour window. The key is consistency, not extremism.
Timing matters significantly. The body is more insulin-sensitive in the morning and early afternoon. Eating late at night forces your body to process glucose when insulin sensitivity is lowest, making glucose more likely to be stored as visceral fat. Finishing your last meal at least 3-4 hours before bedtime allows insulin to fall, cortisol to normalize, and growth hormone to rise during sleep. Growth hormone is one of the most powerful fat-burning hormones, especially for visceral fat.
When breaking a fast, meal composition is critical. Protein and fiber should come first—they stabilize blood sugar, reduce insulin spikes, and support gut health. Starting with highly refined carbohydrates spikes insulin and undoes much of the fasting benefit.
Movement That Lowers Cortisol Rather Than Raising It
The type of movement matters far more than the amount. Chronic endurance exercise, especially when paired with calorie restriction, raises cortisol and reinforces the stress response. The body adapts by conserving energy and protecting visceral fat.
Resistance training is one of the most effective tools for visceral fat loss. When muscles contract against resistance, they pull glucose from the bloodstream without requiring insulin. This alone lowers insulin demand and improves metabolic flexibility. Muscle is a metabolic organ—the more functional muscle you have, the more glucose you can dispose of safely.
Walking deserves special emphasis. Walking lowers cortisol, improves circulation, enhances insulin sensitivity, supports lymphatic flow and digestion, and does all of this without stressing your nervous system. A daily walk, especially outdoors, is one of the most underrated visceral fat-reduction tools available.
Short, intense bursts of activity—sprinting, interval training, or brief uphill walks—can activate fat-burning pathways and improve mitochondrial health when recovery is adequate. These sessions should be brief and infrequent, not daily marathons.
Sleep: The Non-Negotiable Foundation
Poor sleep worsens insulin resistance and raises cortisol. Movement improves sleep quality when done earlier in the day, but late-night intense exercise elevates cortisol and delays melatonin release. Timing matters.
Consistency in sleep timing is metabolically powerful. Going to bed and waking at the same time daily helps regulate circadian rhythms, stabilize cortisol patterns, and optimize fat-burning hormones. Aim for 7-9 hours nightly.
Practical Implementation: The Step-by-Step Framework
Phase 1: Remove Cortisol Triggers (Weeks 1-2)
Before increasing fasting intensity or exercise volume, stabilize your cortisol baseline:
- Establish consistent sleep timing. Go to bed and wake at the same time daily, even weekends.
- Stop eating 3-4 hours before bedtime. This allows insulin to fall and cortisol to normalize overnight.
- Reduce caffeine after 2 PM. Caffeine amplifies cortisol elevation, especially when combined with stress or poor sleep.
- Eliminate screens 1 hour before bed. Blue light delays melatonin release and disrupts sleep quality.
- Add a daily walk. Even 20-30 minutes of easy walking lowers cortisol and improves insulin sensitivity.
Phase 2: Optimize Eating Patterns (Weeks 3-4)
Once cortisol stabilizes, introduce time-restricted eating:
- Choose an 8-hour eating window (e.g., 12 PM to 8 PM or 10 AM to 6 PM). Consistency matters more than the specific window.
- Eat whole foods. Prioritize protein, vegetables, healthy fats, and whole grains. Minimize refined carbohydrates and ultra-processed foods.
- Start meals with protein and fiber. This stabilizes blood sugar and reduces insulin spikes.
- Hydrate during fasting periods. Dehydration raises cortisol. Drinking water supports blood volume and improves fat mobilization.
Phase 3: Add Movement (Weeks 5+)
Once eating patterns are established and sleep is consistent:
- Add 2-3 resistance training sessions per week. Focus on compound movements that engage large muscle groups.
- Continue daily walking. This remains your primary cortisol-management tool.
- Avoid excessive cardio. If you enjoy running or cycling, keep sessions moderate and infrequent.
Common Mistakes That Sabotage Visceral Fat Loss
Stacking stresses simultaneously: The biggest mistake people make is fasting longer, exercising harder, sleeping less, drinking more caffeine, and restricting calories all at once. This combination signals danger to your body, which responds by clinging to visceral fat even more tightly.
Obsessing over perfection: Stressing about food, tracking every calorie, and fearing meals raises cortisol. The body responds by holding on tighter. Calm, predictable routines are metabolically healing.
Ignoring meal timing: Eating late at night disrupts circadian rhythm, increases morning insulin resistance, and promotes visceral fat storage. This single factor undermines other efforts.
Chronic cardio without recovery: Endurance athletes often develop stubborn belly fat because excessive exercise without adequate recovery raises cortisol chronically.
Expecting linear progress: Visceral fat loss isn’t linear. Some weeks the scale won’t move, but metabolic markers improve. Waist circumference may decrease before weight changes. Blood sugar and triglycerides often improve first. These are signs that visceral fat is being mobilized.
When to Seek Professional Guidance
Consult a healthcare provider if you experience:
- Persistent abdominal bloating or discomfort despite dietary changes
- Unexplained weight gain concentrated in the abdomen
- Elevated fasting blood glucose (above 100 mg/dL) or HbA1c (above 5.7%)
- Fatty liver disease confirmed by imaging or elevated liver enzymes
- Severe sleep disturbances unresponsive to lifestyle modifications
- Extreme fatigue or mood changes suggesting hormonal imbalance
A functional medicine practitioner or endocrinologist can assess your insulin levels, cortisol patterns, and metabolic health through appropriate testing and provide personalized recommendations.
The Bottom Line: Hormones, Not Willpower
Visceral fat loss isn’t about fighting your body through willpower and restriction. It’s about working with your body’s hormonal systems. When insulin levels fall, the lock on fat storage opens. When cortisol normalizes, your body no longer feels the need to protect its vital organs with visceral fat. When inflammation resolves and circadian rhythms are restored, metabolism regains its natural rhythm.
This approach produces results that are not only visible but sustainable. You’re not pursuing temporary weight loss—you’re achieving true metabolic recovery.
Your Next Step: Start tonight by setting a consistent bedtime and finishing eating 3-4 hours before sleep. This single change begins normalizing your cortisol rhythm. Comment below which strategy you’re implementing first—I’d love to hear your commitment.
Medical References
- Després, J. P., & Lemieux, I. (2006). Abdominal obesity and metabolic syndrome. Nature, 444(7121), 881-887. https://doi.org/10.1038/nature05488
- Cleveland Clinic – Visceral Fat: What It Is and Why It Matters
- Kuk, J. L., Katzmarzyk, P. T., Nichaman, M. Z., Church, T. S., Blair, S. N., & Ross, R. (2006). Visceral fat accumulation in relation to insulin resistance and hyperinsulinemia. Obesity, 14(12), 2277-2283.
- NIH – Cortisol and Stress Response
- de Cabo, R., & Mattson, M. P. (2019). Effects of intermittent fasting on health, aging, and disease. New England Journal of Medicine, 381(26), 2541-2551.
Disclaimer: This article is for informational purposes only and should not replace professional medical advice. Consult with a qualified healthcare provider before making significant dietary or exercise changes, especially if you have existing health conditions or take medications.