Leaky gut and heart disease may seem like two very different health problems — one tied to the digestive system, the other to the cardiovascular system. Yet modern research suggests these two are closely intertwined, like two pieces of a complex biological puzzle. In fact, scientists are now exploring how a compromised intestinal barrier could play an unexpected role in the development of atherosclerosis, coronary artery disease (CAD), and other serious heart conditions. (OUP Academic)
Let’s unpack the science, the mechanisms, and the real-world implications behind the connection between leaky gut and heart disease in a way that’s both accessible and evidence-based.
What Is a “Leaky Gut”?
Imagine your intestinal lining as a finely woven net — a barrier that lets nutrients in and keeps harmful substances out. Under normal conditions, this barrier does a great job filtering what gets absorbed into your bloodstream. But when this barrier weakens, gaps form between the cells lining the gut. This condition, often referred to as “leaky gut”, allows substances such as bacterial components and toxins to escape from the gut and enter systemic circulation. (PubMed)
In medical research, this phenomenon is more precisely described as increased intestinal permeability. It’s not simply a catchy buzzword — it’s a measurable biological state that can trigger systemic inflammation when harmful molecules like bacterial endotoxins pass through these weakened gaps. (PubMed)
How It Happens
- Tight junction disruption: Tight junction proteins hold the gut lining together. Diet, stress, infection, or medications can weaken them. (PubMed)
- Dysbiosis: An imbalance in gut microbes can degrade the protective mucus layer and compromise barrier function. (PubMed)
- Inflammation: Chronic inflammation itself can further weaken the intestinal barrier, creating a self-perpetuating cycle. (PubMed)
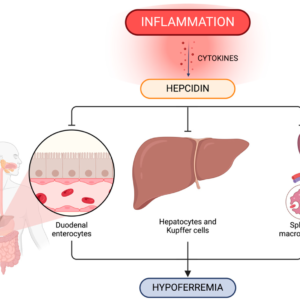
At this point, portions of the debris from gut microbes — like lipopolysaccharides (LPS) from Gram-negative bacteria — can leak into the bloodstream and activate the immune system. (MDPI)

The Science Behind the Gut–Heart Connection
You might be asking: How could bacteria in your intestines possibly affect your heart? The answer lies in chronic inflammation and microbial metabolites that enter systemic circulation when the gut barrier fails.
Bacterial Products in Your Bloodstream
One major influencer is lipopolysaccharide (LPS) — a structural component of certain bacteria. Under normal conditions, LPS stays inside the gut. But when the barrier is compromised, LPS can slip through and enter the bloodstream.
Once there, it triggers immune receptors like Toll-like receptor 4 (TLR4) and promotes the release of inflammatory cytokines such as IL-6 and TNF-α. These molecules are central players in chronic inflammation, and inflammation is a known driver of cardiovascular disease. (MDPI)
Microbial Metabolites That Matter
Beyond LPS, other microbial byproducts can influence heart health:
- Trimethylamine-N-oxide (TMAO): Gut bacteria convert choline and carnitine (from red meat and eggs) into TMA. The liver then turns TMA into TMAO, which has been linked to atherosclerosis and cardiovascular risk. (MDPI)
- Short-chain fatty acids (SCFAs): Produced by beneficial bacteria from fiber, SCFAs can be protective — but an imbalance in microbes often reduces SCFA production. (PubMed)
These circulating microbial components can interact with cholesterol metabolism, immune signaling, and even platelet activity — all key elements in the development of heart disease. (MDPI)
How Leaky Gut May Promote Heart Disease
To truly understand the link, let’s break down the mechanisms through which a leaky gut might contribute to cardiovascular problems.
1. Chronic Low-Grade Inflammation
Systemic inflammation plays a central role in the development of atherosclerosis, the buildup of plaques inside artery walls. Plaque formation is not just a matter of cholesterol — it’s an inflammatory process that involves immune cells responding to perceived threats. (OUP Academic)
When microbial products from the gut repeatedly enter circulation, they stimulate immune receptors and can induce a persistent inflammatory response. Over time, this chronic inflammation may contribute to plaque formation, progression, and instability, which can lead to heart attacks and strokes. (MDPI)
2. Endothelial Dysfunction
The endothelial cells lining blood vessels are essential for vascular health. Persistent inflammation can disrupt their normal function, reducing their ability to dilate properly and control blood pressure. Over time, this stress on the vascular system increases cardiovascular risk.
3. Immune Activation and Plaque Instability
Immune cells that become activated by gut-derived endotoxins can infiltrate arterial walls and contribute to plaque vulnerability. This scenario is similar to what happens in chronic infections — the immune system becomes more reactive, and plaques become more unstable and prone to rupture. (ScienceDirect)
Evidence From Research
Although this area of research is still evolving, a growing body of scientific evidence supports the gut–heart connection.
Scientific Findings
- A review in the European Heart Journal noted that patients with conditions featuring increased intestinal permeability often show heightened risk for coronary heart disease — even when traditional risk factors are not present. (OUP Academic)
- Research suggests that gut microbiota dysbiosis and metabolic byproducts like TMAO may directly impact lipid transport, inflammation levels, and plaque development. (MDPI)
- A comprehensive review in PubMed Central highlighted the role of impaired intestinal barrier function as a predictive factor for adverse cardiovascular outcomes, including hypertension and coronary artery disease. (PubMed)
While more clinical trials are needed, the existing data strongly support a gut-to-heart axis — a communication pathway where gut health influences cardiovascular health.
A Simple Comparison: Healthy vs. Leaky Gut Scenarios
| Feature | Healthy Gut | Leaky Gut |
|---|---|---|
| Intestinal Barrier | Strong, tight junctions intact | Weakened with increased permeability |
| LPS in Blood | Low | Elevated |
| Chronic Inflammation | Minimal | Persistent |
| Cardiovascular Risk | Lower | Higher |
| Microbial Metabolites (TMAO, SCFAs) | Balanced | Imbalanced |
| Atherosclerotic Progression | Slower | Accelerated |
This table gives a clear snapshot at a glance of how gut integrity may influence cardiovascular risk.
Signs That May Point to a “Leaky Gut”
While only clinical testing can confirm increased intestinal permeability, certain symptoms and conditions have been associated with gut barrier issues:
- Digestive discomfort, bloating, or irregular bowel habits
- Autoimmune disorders or frequent infections
- Chronic fatigue or unexplained inflammation
- Elevated inflammatory markers on blood tests
Although leaky gut is not yet a formal diagnosis in conventional medicine, increased intestinal permeability is a measurable phenomenon with growing clinical interest. (PubMed)
Can Improving Gut Health Reduce Heart Risk?
Here’s where things become actionable. If the gut–heart connection is real (and evidence suggests it is), then supporting gut integrity may be one way to reduce cardiovascular risk.
Dietary Strategies
Certain foods have been shown to help maintain or restore gut barrier function:
- High-fiber foods: Feed beneficial bacteria and boost SCFA production.
- Fermented foods: Provide probiotics that support a balanced microbiome.
- Plant-based nutrients: Polyphenols from berries, green tea, and olive oil help reduce inflammation.
On the flip side, diets high in saturated fats, sugars, and processed foods have been linked with dysbiosis and increased intestinal permeability.
Lifestyle Factors
- Regular exercise: Linked with greater microbial diversity and improved gut integrity.
- Stress management: Chronic stress may weaken barrier function through hormonal effects.
- Adequate sleep: Supports immune regulation and gut health.
Emerging therapies even include probiotics, prebiotics, and targeted microbial metabolite modulation — but more human studies are needed before broad recommendations can be made.
For an in-depth exploration of gut microbiota’s role in cardiovascular disease, see this scientific review on gut microbiota and cardiovascular health. (MDPI)
The Bottom Line
The connection between leaky gut and heart disease might once have sounded surprising, but it’s becoming harder to ignore. Emerging research highlights how compromised intestinal barrier function, gut microbial products, and chronic inflammation can fuel the development and progression of cardiovascular diseases. (OUP Academic)
While traditional risk factors like high blood pressure and cholesterol remain important, gut health adds another layer to our understanding of heart disease — one that’s revealing new opportunities for prevention and holistic care.