(Read This First)
For over 20 years, millions of women were quietly steered away from estrogen therapy—based on a misunderstanding so massive it reshaped modern medicine.
What if the “risk” you were warned about was never the real danger at all?
Introduction: Why Estrogen Therapy in Menopause Became So Controversial
Estrogen therapy in menopause didn’t fall out of favor because it failed women.
It fell because medicine failed to interpret its own data.
In the 1970s and 1980s, prescribing estrogen during menopause was standard practice. Doctors saw women sleep better, think clearer, protect their bones, and regain quality of life. Then came a single study—the Women’s Health Initiative (WHI)—and everything changed.
Almost overnight, estrogen therapy was branded dangerous.
Doctors panicked. Headlines screamed. Women were pulled off hormones mid-treatment. And menopause became something women were told to “just endure.”
But here’s the uncomfortable truth: the conclusions were flawed, and the consequences were enormous.
Let’s unpack what actually happened—and what modern science now understands.
Estrogen Therapy Menopause: How Female Hormones Actually Work
To understand estrogen therapy risks and benefits in menopause, we need to start with biology—not fear.
From puberty to menopause, a woman’s hormones follow a beautifully orchestrated rhythm:
- Estrogen rises in the first half of the cycle, preparing ovulation
- Progesterone dominates the second half, stabilizing mood and supporting pregnancy
- Both hormones drop sharply before menstruation
This cycle repeats hundreds of times over decades.
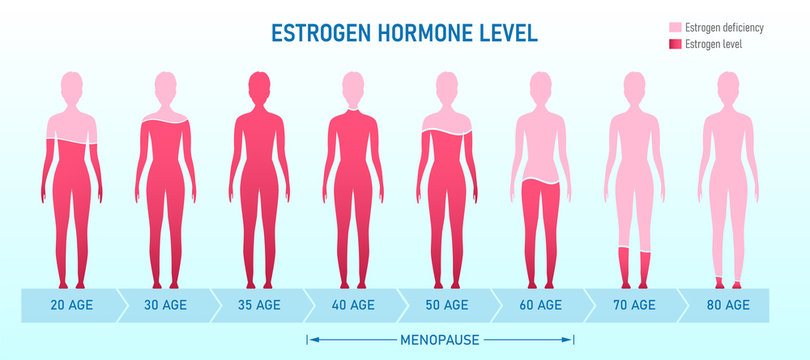
What Changes During Menopause?
Menopause isn’t just “no more periods.” It’s a hormonal shutdown.
Estrogen levels fall dramatically, triggering:
- Hot flashes and night sweats
- Sleep disruption
- Brain fog
- Vaginal dryness
- Bone loss (osteopenia → osteoporosis)
- Increased cardiovascular risk
Estrogen receptors exist in the brain, bones, blood vessels, skin, and heart. When estrogen disappears, the body notices—everywhere.
That’s why estrogen therapy in menopause was originally considered logical, compassionate care.
The Women’s Health Initiative: Medicine’s Biggest Hormone Mistake
If estrogen therapy helps, why did the medical world abandon it?
Enter the Women’s Health Initiative (WHI)—often cited as the study that “proved” hormone therapy was dangerous.
But here’s what most headlines left out.
Who Was Studied (And Why That Matters)
The WHI didn’t study women starting hormones at menopause.
Instead, it enrolled women who were:
- 10–20 years post-menopause
- Mostly over 63 years old
- High rates of obesity, smoking, diabetes
- Largely asymptomatic
This is like testing seatbelts only in car crashes at 120 mph and concluding seatbelts are unsafe.
The Hormones Used Were Outdated
The study used:
- Conjugated Equine Estrogen (CEE) — derived from horse urine
- Medroxyprogesterone Acetate (MPA) — a synthetic progestin
Modern estrogen therapy menopause protocols use bioidentical estradiol patches and micronized progesterone, which behave very differently in the body.
Estrogen Therapy Risks & Benefits: The Breast Cancer Myth
This is where fear took over science.
The Headline Everyone Remembered
“Hormone therapy increases breast cancer risk by 26%.”
Sounds terrifying—until you see the actual numbers.
Absolute Risk vs Relative Risk (The Trick You Were Never Taught)
| Measure | Result |
|---|---|
| Relative risk increase | ~26% |
| Absolute risk increase | 1 extra case per 1,000 women |
Going from 4 in 1,000 to 5 in 1,000 became global panic.
Even more interesting?
- Women on estrogen-only therapy (no uterus) showed a lower breast cancer rate
- Risk signals pointed more strongly toward synthetic progesterone, not estrogen
This distinction matters—and it was largely ignored.
For a deeper breakdown of risk interpretation, Harvard Medical School explains this clearly in their analysis on absolute vs relative risk in hormone therapy
👉 https://www.health.harvard.edu/powerful-numbers-absolute-risk-vs-relative-risk
Modern Estrogen Therapy Menopause Benefits (What We Know Now)
When started at the right time, using the right formulation, estrogen therapy offers profound benefits.
Documented Benefits of Estrogen Therapy in Menopause
- Reduced hot flashes and night sweats
- Improved sleep quality
- Stronger bones and reduced fracture risk
- Improved insulin sensitivity
- Reduced cardiovascular disease risk (when started early)
- Better cognitive clarity
- Improved vaginal and urinary health
The concept is now called the “timing hypothesis”—start estrogen close to menopause, not decades later.
The Cleveland Clinic provides a clear overview of these benefits here:
👉 https://my.clevelandclinic.org/powerful-menopause-hormone-therapy-benefits
Bioidentical Estrogen Therapy: Why Delivery Method Matters
Not all estrogen therapy is equal.
Oral Estrogen (Old School)
- Passes through the liver
- Increases clotting factors
- Slightly raises stroke risk
Transdermal Estrogen (Modern Gold Standard)
- Absorbed through the skin
- Bypasses the liver
- Lower clot risk
- More stable hormone levels
This is why estrogen patches, gels, and creams dominate modern menopause care.
Progesterone: The Unsung Hero (and Villain for Some)
If a woman has a uterus, progesterone is required to protect against uterine cancer.
The Catch?
Not all women tolerate progesterone well.
Some experience:
- Mood swings
- Anxiety
- Depression
For these women, doctors now use progesterone-coated IUDs, delivering local protection without systemic side effects.
Ironically, progesterone also eliminates PMS symptoms in many women—highlighting how individual hormone sensitivity truly is.
Estrogen Therapy Menopause vs Testosterone Therapy for Women
Here’s a fact that surprises almost everyone:
Women have more testosterone than estrogen in absolute quantity—just at far lower levels than men.
When Testosterone Therapy Is Considered
- Extremely low testosterone levels
- Low libido
- Difficulty maintaining muscle mass
Used carefully and within physiological ranges, low-dose topical testosterone can be helpful.
What it does not cause at proper doses:
- Facial hair growth
- Voice deepening
- Clitoral enlargement
The data is still evolving, which is why testosterone therapy for women remains cautious and individualized.
Estrogen Therapy Risks & Benefits: A Balanced Comparison
| Factor | Estrogen Therapy | No Hormone Therapy |
|---|---|---|
| Hot flashes | ↓ Significant | Persistent |
| Bone loss | ↓ Reduced | Accelerated |
| Heart disease risk | ↓ If early | Increases |
| Breast cancer risk | Neutral to slight ↑ | Baseline |
| Quality of life | Improved | Often impaired |
Context—not fear—should guide decisions.
Who Should Avoid Estrogen Therapy in Menopause?
Estrogen therapy isn’t for everyone.
It may be avoided in women with:
- Active estrogen-sensitive breast cancer
- Uncontrolled clotting disorders
- Severe liver disease
That said, blanket avoidance harms more women than it protects.
Individual risk assessment beats outdated dogma every time.
The Human Cost of Fear-Based Medicine
One unintended consequence of the WHI fallout?
A generation of women told:
- “Suffering is normal”
- “Hot flashes are just part of aging”
- “Brain fog is inevitable”
That narrative stole quality of life from millions.
Menopause isn’t a moral test of endurance.
It’s a biological transition—one modern medicine can support intelligently.
Final Thoughts: Estrogen Therapy Menopause Deserves a Rethink
Estrogen therapy risks and benefits in menopause were never about absolutes.
They were about:
- Timing
- Formulation
- Individual biology
When done correctly, estrogen therapy is not reckless—it’s restorative.
The real danger wasn’t estrogen.
It was misunderstanding data, magnifying fear, and silencing nuance.