(Read This First)
High blood pressure isn’t bad luck.
It’s your body waving a red flag and begging you to listen.
For decades, we’ve been told hypertension is “essential,” permanent, and best managed with pills for life. But what if that story is incomplete—and dangerously misleading?
Introduction: Why High Blood Pressure Is Widely Misunderstood
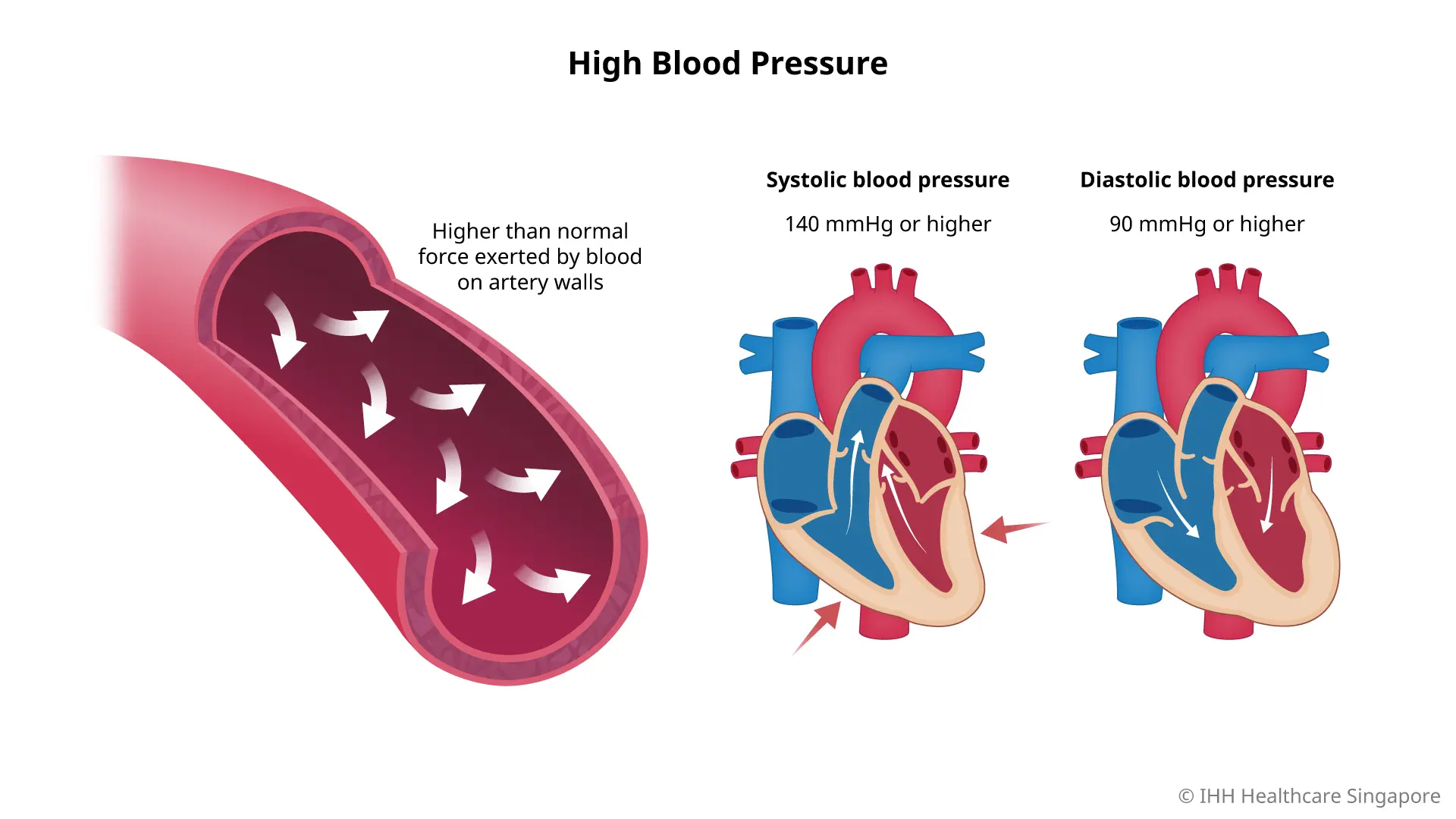
High blood pressure, clinically known as hypertension, has quietly become a global epidemic. More than half of adults worldwide now fall into the hypertensive or pre-hypertensive category. Yet despite how common it is, hypertension remains one of the most misunderstood medical conditions of our time.
Traditionally, doctors are taught that 95% of high blood pressure cases are “primary” or “essential” hypertension, meaning no clear cause can be identified. The remaining 5% are blamed on obvious culprits like kidney disease or rare tumors. Once the label is applied, the prescription pad comes out, and the conversation often ends there.
But cardiologist Dr. Pradip Jamnadas challenges this narrative head-on. Drawing from years of clinical experience, he argues that there is nothing “essential” about high blood pressure. In fact, for many patients, hypertension is not a disease—it is a symptom of deeper metabolic dysfunction.
And here’s the hopeful part: symptoms can be reversed.
High Blood Pressure and End-Organ Damage: The Real Stakes
High blood pressure is dangerous not because of the numbers on the cuff, but because of what those numbers do over time.
Unchecked hypertension silently damages vital organs, often long before symptoms appear.
The organs most at risk include:
- Heart – heart attacks, heart failure, thickened heart muscle
- Brain – strokes, vascular dementia
- Eyes – retinal damage and blindness
- Kidneys – chronic kidney disease and failure
- Blood vessels – atherosclerosis and arterial stiffness
According to the American Heart Association, hypertension is a leading contributor to preventable death worldwide. You can explore their life-saving insights through this powerful evidence-based guide on blood pressure risks:
👉 https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure
The tragedy is that most of this damage occurs silently. Many patients feel “fine” until a major event happens. That’s why controlling high blood pressure is critical—but understanding why it exists is even more important.
The Myth of “Essential” Hypertension
The term essential hypertension sounds official, but it hides a troubling truth: it often means “we didn’t look deep enough.”
Medical training historically taught that high blood pressure just “happens” with age, genetics, or stress. While these factors play a role, they rarely tell the full story.
Dr. Jamnadas emphasizes that labeling hypertension as essential shuts down curiosity. Once a condition is declared permanent, both patients and doctors stop asking the most important question:
What is driving this?
Over time, clinical observation has revealed something remarkable—many patients who address underlying metabolic issues can reduce or completely eliminate their need for blood pressure medication.
That discovery turns decades of conventional wisdom upside down.
Metabolic Syndrome and High Blood Pressure: The Missing Link
What Is Metabolic Syndrome?
Metabolic syndrome is not a single disease. It’s a cluster of interconnected metabolic abnormalities that dramatically increase the risk of heart disease, diabetes, and high blood pressure.
The core features include:
- High blood pressure
- Elevated triglycerides
- Low HDL (“good”) cholesterol
- Increased waist circumference (belly fat)
- Insulin resistance
More than 50% of adults now meet the criteria for metabolic syndrome, whether they realize it or not.
To understand how deeply metabolism affects blood pressure, research from the National Institutes of Health highlights the dangerous cascade of insulin resistance and vascular dysfunction:
👉 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6571271/
This isn’t fringe science. It’s mainstream, well-documented physiology.
Why Obesity Is a Symptom, Not the Root Cause
One of the most misunderstood aspects of hypertension is its relationship with weight.
Yes, many people with high blood pressure are overweight—but weight gain is often the result of metabolic dysfunction, not the cause.
Here’s what the data shows:
- About 80% of overweight individuals have metabolic syndrome
- Roughly 20% of people with metabolic syndrome are not overweight
These individuals are often described as TOFI — Thin Outside, Fat Inside. They may look healthy but carry dangerous visceral fat around their organs.
In these cases, focusing solely on weight loss misses the bigger picture. The real problem lies in hormonal imbalance, particularly elevated insulin levels.
How Insulin Resistance Drives High Blood Pressure
The Hormonal Explanation Doctors Rarely Share
Insulin isn’t just a blood sugar hormone. It also affects how your blood vessels function.
When insulin levels remain chronically high—a condition known as insulin resistance—blood vessels lose their ability to relax properly. This causes persistent narrowing of the arteries, leading directly to high blood pressure.
In simple terms:
- High insulin → stiff arteries
- Stiff arteries → higher pressure
- Higher pressure → organ damage
This explains why traditional “eat less, move more” advice often fails. The problem isn’t calories—it’s hormones.
The calorie-in, calorie-out model has been thoroughly debunked, yet it continues to dominate public health messaging.
Why Blood Pressure Pills Alone Are Not Enough
Medication absolutely has a role, especially when blood pressure is dangerously high. But pills treat the symptom, not the source.
A truly complete hypertension workup should include:
- Fasting insulin levels
- Triglyceride-to-HDL ratio
- Inflammatory markers
- Liver function tests (fatty liver screening)
- Sleep apnea evaluation
Without these data points, doctors are essentially managing numbers instead of restoring health.
Sleep Apnea and High Blood Pressure: A Dangerous Duo
Sleep apnea often flies under the radar, yet it plays a major role in stubborn hypertension.
Repeated oxygen deprivation during sleep triggers stress hormones that keep blood pressure elevated around the clock. While obesity increases risk, even lean individuals can suffer from sleep apnea.
Addressing sleep quality alone can lead to dramatic improvements in blood pressure control.
How to Reverse High Blood Pressure Naturally
The Lifestyle Strategy That Actually Works
Dr. Jamnadas reports removing hundreds of patients from blood pressure medications by addressing metabolic health first.
The approach is surprisingly simple—but not easy.
Core principles include:
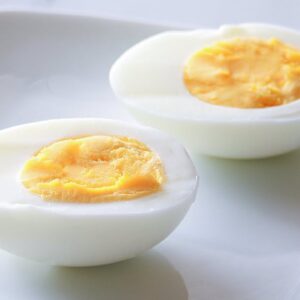
- Eating whole, unprocessed foods
- Eliminating refined sugars and artificial ingredients
- Prioritizing protein, healthy fats, and fiber
- Practicing intermittent fasting or time-restricted eating
Intermittent fasting is particularly powerful because it restores insulin sensitivity, allowing hormone levels to normalize naturally.
As insulin levels drop, arteries relax. As arteries relax, blood pressure falls.
Weight loss follows—not because of calorie restriction, but because metabolism heals.
Table: Conventional vs Metabolic Approach to High Blood Pressure
| Approach | Focus | Long-Term Outcome |
|---|---|---|
| Conventional Care | Blood pressure numbers | Lifelong medication |
| Metabolic Approach | Insulin, inflammation, hormones | Potential reversal |
| Calorie Restriction | Weight loss | Often temporary |
| Hormonal Balance | Insulin sensitivity | Sustainable results |
Why Hypertension Is Not the End of the Road
A diagnosis of high blood pressure is not a life sentence. It’s a wake-up call.
It signals that something deeper is out of balance—and that imbalance is often reversible.
When patients shift from asking “Which pill do I need?” to “Why is my body doing this?”, everything changes.
Healing becomes possible.
Key Takeaways (Read This Twice)
- High blood pressure is often a symptom, not a disease
- Metabolic syndrome is a major hidden driver of hypertension
- Insulin resistance stiffens arteries and raises blood pressure
- Weight gain is often hormonal, not caloric
- Lifestyle changes can restore normal blood pressure in many cases
Conclusion: Control the Cause, Not Just the Numbers
High blood pressure doesn’t appear overnight. It develops slowly, quietly, and often invisibly. But it doesn’t have to be permanent.
By addressing metabolic health, insulin resistance, sleep quality, and lifestyle factors, many people can dramatically reduce—or even eliminate—their reliance on medication.
The real work begins when you stop managing symptoms and start restoring balance.
Your body isn’t broken.
It’s communicating.
Call to Action
👉 Read More
👉 Share Now